Successful fluid resuscitation in the acute or critical setting is a crucial step in patient stabilization. The nurse practitioner (NP) who is well-versed in the most current principles governing fluid resuscitation can therefore move confidently during critical situations. By the end of this session, the NP will be able to identify the pathophysiological complications associated with ineffective volume resuscitation in the acutely ill or injured, describe the relevant physiological endpoints for determining euvolemia in various patient populations, and confidently use multiple strategies to optimize resuscitation.
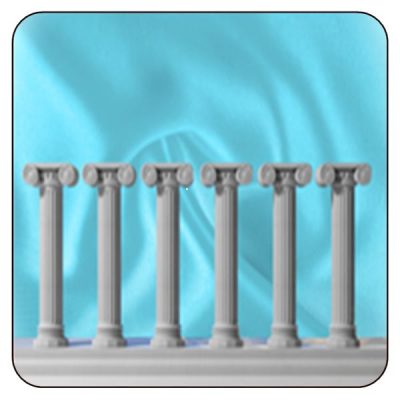
This offering is structured around six pillars of fluid resuscitation, which are defined as follows:
- Fluid responsiveness is foundational to resuscitation.
- Central venous pressure (CVP) and vena cava measurement are not the sole indicators for determining fluid responsiveness.
- An accurate reading of fluid responsiveness can be gained by using the passive leg raising maneuver in tandem with the stroke volume index.
- A fluid challenge ordinarily produces a small and brief hemodynamic response.
- Fluid responsiveness does not always necessitate a fluid bolus.
- An elevated CVP should be strongly considered in relation to compromised organ perfusion.
Sample